#
As Ontario continues to grapple with the impacts of COVID-19, the importance of integrating health care and social supports is more critical than ever. While it is heartening to hear so many stories of informal community care, mutual aid and caremongering already underway across local communities, we must act now to ensure that these important gains continues to be deepened and strengthened in formal healthcare and community support delivery.
Read our media release: Ontario’s Social Prescribing pilot project shows strength of community health interventions to systemically address social impacts of COVID-19 measures
***
#Rx: Community- Social Prescribing Research Pilot
September 2018 marked the launch of an exciting chapter at Alliance as we initiated a first-of-its-kind pilot project in Ontario, called Rx: Community – Social Prescribing. As we learned about the core values of social prescribing, we realized that the Alliance shared the same values on which social prescribing operates from. Both our organization and this model of care apply a comprehensive approach to health and wellness, that is seeing health as grounded in community, and recognize the importance of empowering clients to act as partners in their care.
To help advance Rx: Community’s success, it was important that we form key partnerships with well-experienced professionals within the field of social prescription. We successfully partnered with mentors from the UK - Herts Valley Clinical Commissioning Group, experienced in social prescribing navigation, and Altogether Better, an organization with expertise in co-creation between primary care staff and clients.
We began Rx: Community with an invitation to our member centers for an introductory session in order to learn how their work can align with the principles of social prescribing. From this session, 11 of our members, representing a diverse mix of urban, rural, Northern, and francophone communities, expressed interest in implementing social prescribing in their day-to-day practices. Some of the unique features our pilot program were the application of an equity-based lens in our approach to providing care. We ensured that material support was provided for our clients through food programs, housing, etc., as well as prescribing social prescribing champions – clients who co-designed and led programs for other clients to attend. From the lovely tunes of orchestra harmonies to delectable tastes of locally grown fresh produce, Rx: Community has offered a multitude of care treatments through social interventions and community referrals from our participating member centers. A key takeaway from this pilot project is recognizing that social prescribing may look different in different communities, depending on local needs and capacity.


Positive impacts on individuals, healthcare providers, and system integration
Rx: Community used a combination of different approaches to examine how social prescribing was implemented. Through client and provider surveys, focus groups, and health records, we tracked the impact of our work to understand how social prescription affected clients’ sense of wellbeing, health outcomes, and use of the health system. Additionally, we observed positive effects of social prescribing on the prescribers’ work and confidence as a result of their clients’ positive feedback. During the year-long pilot, over 1,100 clients across 11 CHCs were provided a total of nearly 3,300 social prescriptions. Seventy-one of the clients who received social prescriptions were supported to become volunteer Health Champions who co-created and delivered social activities and programs.
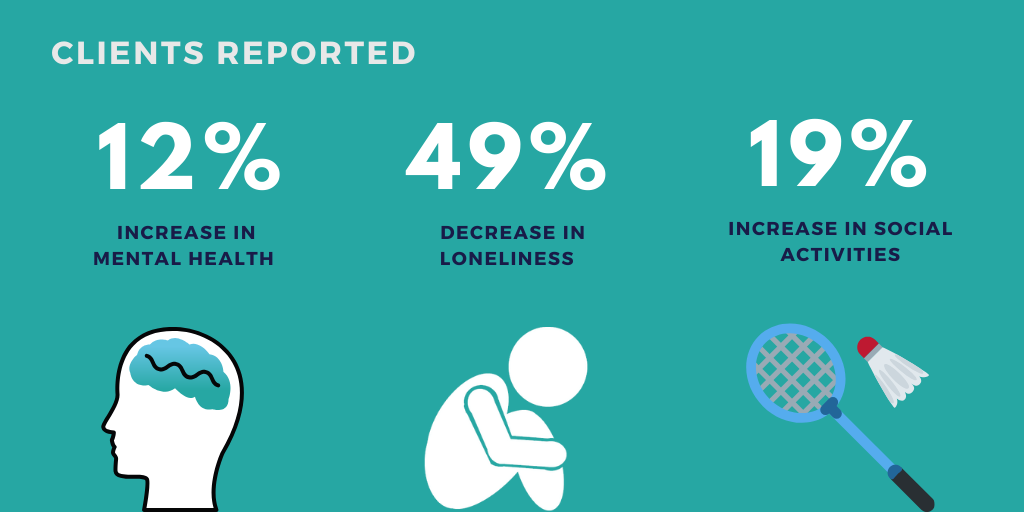
- Finding #1: Clients reported overall improvements to their mental health and a greater capacity to self-manage their health, as well as decreased loneliness and an increased sense of connectedness and belonging.
- Finding #2: Healthcare providers find social prescribing useful for improving client wellbeing and decreasing repeat visits. They recognized the value of the navigator role, and, where it was not in place, they felt a need for more support.
- Finding #3: Social prescribing enabled deeper integration between clinical care, interprofessional teams, and social support, and it enhanced the capacity of the community through co-creation.

Watch this introductory video on social prescribing:
Read the final report:
- Rx: Community - Social Prescribing in Ontario Final Report, March 2020 (+ COVID-19 Letter)
- Rx: Communauté - Rapport final sur la Prescription Sociale en Ontario, Mars 2020 (+ COVID-19 lettre)
#What’s next?
Social prescribing is gaining momentum in Canada among healthcare providers, community partners, researchers, funders, and policymakers. The wide interest and promising findings from Rx: Community shows that we ready to scale social prescribing broadly to support a more integrated health system and build more connected communities.
We recommend that:
- Policymakers, funders, and Ontario Health Teams can create fertile ground for social prescribing by investing in primary health care and social supports. They can further advance social prescribing initiatives with direct financial, material, and/or policy support.
- Health care, cross-sectoral, and social support organizations can build and strengthen local partnerships, adapt social prescribing to the needs and assets of their communities, embrace culture change, and develop strategies for data collection and use.
- Researchers and academic institutions can contribute screening and evaluation tools, conduct data analysis, and provide research support to health care and social support organizations.
#Key Resources
- Rx Community - Social Prescribing in Ontario Final Report, March 2020 (Résumé en français)
- Rx: Community - Social Prescribing in Ontario, Progress Report, June 2019 ( English | French )
- Social Prescribing Media Release ( English | French )
- Social Prescribing Backgrounder ( English | French )
Looking for something older? Check out our Rx: Community Library.
#In the Media
- Social prescribing: The next step for equitable healthcare, Healthy Debates, August 20, 2020
- For people living alone, quarantines and physical distancing present unique challenges, The Globe and Mail, April 21, 2020
- Social prescribing in the age of COVID-19, Upstream, April 15, 2020
- Prescriptions are for more than just drugs. Ontario Health Teams should use ‘social prescribing’ to improve our health and wellbeing, Healthy Debates, February 6, 2020
- 'It changed my life': New pilot project tests health benefits of social prescribing, CBC, December 24, 2019 (French)
- The cost of loneliness: Canadians are facing a solitary future — and it's affecting their health, Ottawa Citizen, December 19, 2019
- A doctor's prescription for social activities can have great personal and public health benefits (audio link), CBC Metro Morning, November 19, 2019
- Interview with John Paton, social prescribing participant at Belleville & Quinte-West CHC (audio link), CBC Ontario Morning, November 20, 2019
- Marginalized people need social connections, too, Toronto Star, November 11, 2019
- Let’s Wage a War on Loneliness, The New York Times, November 9, 2019
- Guelph doctors, health providers treat loneliness by prescribing yoga and crochet lessons, CBC News, August 14, 2019
- Pilot project has health team prescribing hobbies, social activities to patients, Collingwood Today, July 18, 2019
- Social prescriptions: Sense of belonging could be best medicine (video link), Global News, June 19, 2019
- Analysis: How to find friends in the age of loneliness, YorkRegion.com, April 9, 2019
- New Social Prescribing Pilot Comes to Ontario, Health Quality Ontario Quorum, April 1, 2019
- Better Health Care through Innovation, TVO - The Agenda, March 4, 2019
- Loneliness: the silent killer, University Affairs, February 27, 2019
- Feeling isolated? You can now be prescribed a trip to the museum, Toronto Star, January 28, 2019
- A prescription for happiness, Belleville Intelligencer, January 3, 2019
- 'Social prescriptions' aim to ease patients' depression, loneliness, CBC and CTV News (alternate link), January 1, 2019
- Ontario health-care providers explore social prescriptions to help patients heal without drugs, The Globe and Mail, December 17, 2018
- Doctor's orders: 'Social prescriptions' have been shown to improve health, CBC, December 9, 2018
- Editorial: Forget the pills, play bingo, The Hamilton Spectator, December 9, 2018
- Doctors can now issue prescriptions for free visits to the ROM, blogTO, December 6, 2018
- Doctors can now prescribe a visit to the ROM through a new initiative to combat anxiety and loneliness, Toronto Star, December 6, 2018
- Primary care providers exploring value of “social prescriptions” for patients, Canadian Medical Association Journal News, November 22, 2018
- How social prescribing is changing healthcare in Ontario, Establish Media, November 1, 2018
- Why doctors are prescribing bingo, not pills, to keep patients healthy, CBC, September 30, 2018
- Social prescribing (audio link), CBC Ottawa Morning, September 26, 2018
For more information:
Alliance for Healthier Communities
communications@allianceon.org
Funded by the Ontario Ministry of Health and Long-Term Care
 The views expressed in the publication are the views of the Recipient and do not necessarily reflect those of the Province.
The views expressed in the publication are the views of the Recipient and do not necessarily reflect those of the Province.
